Infectious Diseases Requisition Form (IDR)
These forms were designed to be downloaded and accessed with an Adobe PDF reader (ex: Adobe Acrobat Reader DC). Please be aware that completing the form using a browser’s default PDF reader can create discrepancies in the date fields.
DOH-4463 Infectious Disease Requisition Form Updated 7/2022[1]
DOH-4464 Non-Human Samples Infectious Disease Requisition Form Updated 7/2022[2]
General Instructions
- Enter the full name, date of birth, and county of the patient. If available, include the submitter’s reference number.
- Fill in the submitting laboratory’s name, address, laboratory permitted facility identification (PFI) number, contact person, and phone number.
- Record the specimen collection date, time (if applicable), and source/specimen type.
- Exposure, relevant travel, suspected organism, and all known clinical information should also be completed.
- Place the IDR in the pocket of the transport bag when shipping the specimen. If a specimen is sent without an IDR, testing will not be completed until the required information becomes available to the Wadsworth Center.
Items marked with an asterisk * indicate required information for testing.
Shipping specimens using Courier services is preferred for most infectious disease testing at Wadsworth Center. Courier services MUST be used for shipments of Category A organisms (i.e.
TB), expedited test requests or those being directed to the Biodefense and Viral Diseases Laboratories. Please use the indicated courier address and note the specified Courier Address
listed for shipping specimens to the Rabies Virus Laboratory. Rabies samples not addressed to the Slingerlands Courier address will result in a testing delay.
Refer to the Wadsworth Center Test Catalog on the Health Commerce System (HCS) for test-specific shipping information or call with questions (518-474-4177).
Program Specific Instructions
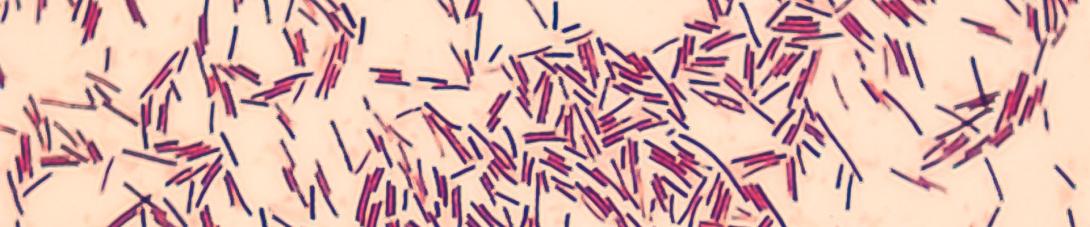
- Bacteriology: None
- Parasitology: Under Clinical and Exposure History, please include travel history when known or indicate unknown. Please note drug susceptibility is currently performed if requested and only on samples containing P. falciparum. Specimens with a very low parasitemia may not be suitable for susceptibility testing.
- Serology: Please be sure to complete the Clinical and Exposure History section.
- Mycology (Fungal): None
- Mycobacteriology: Please complete a separate IDR form for each specimen, if specimens from the same patient were collected on different days / at different times.
- Virology: Please be sure to complete the Clinical and Exposure History section. Influenza antiviral susceptibility testing is available on a case-by-case basis. Please provide details, including specific antiviral, duration and an explanation of why resistance is suspected. Out-of-season requests for arbovirus testing requires relevant explanations to avoid canceled or delayed testing. Provide current and alternate contact information to receive critical test results.
- HIV/HCV: For HIV, please complete race, ethnicity, current gender identity, ordering medical provider’s full name, address and National Provider Identifier (NPI) as per New York State requirements for HIV reporting. For Pediatric HIV Testing, complete the additional required information in the Clinical and Exposure History section. For HIV-2 RNA testing, indicate Qualitative (diagnostic) or Quantitative (viral load). For rapid test confirmation, also check HIV diagnostic testing or HCV RNA, as appropriate, and enter the rapid test type in ‘Submitter Lab Findings’. If applicable, enter relevant treatment (e.g. ARV treatment, PrEP) and pregnancy status with trimester in the appropriate Clinical and Exposure History fields.
- Other: Referral testing, please list organism and include any additional paperwork required (i.e. CDC 50.34 Specimen Submission Form https://www.cdc.gov/infectious-diseases-labs/php/submission-form/index.html[3]
Patient Information
Patient Name, DOB and Sex: patient first and last name OR the submitter’s patient reference number AND date of birth (DOB) in MM/DD/YYYY format. Identifiers must match labels on all specimen containers. (required)
Patient Reference #: a unique identification number for the patient - i.e., a medical record number (MRN). This is NOT a social security number.
NYS DOH Outbreak #: include if the patient is part of an outbreak and a specific number has been assigned by state or local officials.
CDESS (Communicable Disease Electronic Surveillance System) Case #: include if one has been assigned by state or local officials.
Patient Address: patient’s permanent street address. County and State are required fields. Facility of Residence should be included ONLY if the patient resides at a facility other than an individual home or apartment, (i.e. a nursing home or other congregate living setting), at the time of illness.
Race, ethnicity, gender identity: provide patient race, ethnicity, and current gender identify, if available. Specify Asian, Native Hawaiian or Pacific Islander subgroups: Asian Indian, Bangladeshi, Burmese, Cambodian, Chinese, Fijian, Filipino, Guamanian, Hawaiian, Hmong, Indonesian, Japanese, Korean, Laotian, Malaysian, Nepalese, Pakistani, Samoan, Sri Lankan, Taiwanese, Thai, Tibetan, Tongan, Vietnamese, or Other Asian or Pacific Island group, if available.
Occupation/employer: details of patient’s occupation and employer, if available.
Submitter Information – This section must be completed in its entirety
Submitting Facility Name and Address: name and address of the facility/laboratory shipping the specimen(s) to Wadsworth Center for testing. Note: if neither a submitting address nor a PFI is included on the IDR, a laboratory report CANNOT be sent.
Laboratory PFI: Permanent Facility Identifier – ID number for NYS permitted clinical laboratories – include, if applicable. Facility NPI: see NPI below.
Facility Contact Person: name, email, and telephone number of the most appropriate individual to answer questions about the specimens and/or shipment details.
Ordering Healthcare Provider: name and contact information for the healthcare provider requesting testing. Note: this does not have to be the patient’s primary care physician.
NPI (National Provider Identifier): unique 10-digit identification number issued to health care providers in the United States by the Centers for Medicare and Medicaid Services (CMS).
Specimen Information
Collection Date: date of specimen collection in MM/DD/YYYY format. (required)
Time Collected: time of specimen collection, if applicable and available.
Date of Symptom Onset: date on which symptoms began in MM/DD/YYYY format. This is particularly important for the performance of some tests; please refer to the Test Catalog.
Specimen Source: type of material being submitted for testing or from which an isolate being submitted was generated. Use multiple lines if submitting more than one specimen. Examples include, but are not limited to: blood, serum, stool, sputum or bronchial aspirate. (required)
Specimen Type: Isolate refers to a subpopulation, generated from any primary clinical material. Isolate examples include bacterial cultures or cultured viral isolates. Primary specimen refers to original clinical material, directly collected from the patient. Please indicate for each specimen submitted.
Autopsy Specimen: select if the specimen(s) were collected postmortem.
Submitted On/In: if applicable, include any media, preservative or cell line in which the submitted specimen has been collected or in which it is being transported.
Submitter’s Specimen Identifier: identifying number assigned by the laboratory submitting the specimen.
Laboratory Examination Requested
Confirmation: select if testing is being requested in order to confirm results, including specimens sent as required by the NYS Laboratory Reporting of Communicable Diseases Guidelines.
Identification/Detection: select if testing is being requested for the identification or detection of an unknown or suspected microorganism(s) or the antibody response.
Submitter Lab Findings: list all appropriate laboratory examination findings, including the method used to obtain results.
Test Request by Program (suspect organism/agent): select the program(s) in which testing is being requested. Check the box to the left of the specific program AND list any suspected
organism(s)/agent(s) on the line to the right. Note: please do not check more than one laboratory unless testing is being requested in more than one program. Please refer to the Test
Catalog for details on tests offered
Clinical and Exposure History
Relevant Exposures: details including dates for relevant exposures including travel, contact with a known case, animal, arthropod, or food/water exposures. Note: exposure details and prior authorization may be required for some testing, please refer to the Test Catalog. Travel details, including location and dates are requested for: malaria, arboviruses (i.e. dengue virus, chikungunya virus, Zika virus), MERS coronavirus and novel influenza testing.
Relevant Treatments: relevant treatment details, including dates.
Relevant Immunizations: relevant immunization details, including dates. This MAY be important for some test interpretations.
Symptoms, hospital status and other clinical details: list pregnancy status, diagnosis, maximum temperature and ALL notable symptoms. If the patient is hospitalized, please list the hospital with admission dates and ICU status. If CSF was collected, provide Glu, Prot, RBC, and WBC values.